Diabetic retinopathy
Diabetic retinopathy is one of the leading causes of visual loss and blindness.
Diabetic retinopathy
in France
50 % of Type 2 diabetics
1.5 million
patients
Patho physiology of diabetic retinopathy
Diabetes is a disease characterized by chronic hyperglycemia (abnormal levels in blood sugar). This hyperglycemia causes chronic inflammation of the retinal capillaries that results in their occlusion.
Widespread capillary occlusion leads to retinal ischemia due to insufficiency of blood supply in the retina.
Retinal ischemia, when advanced can lead to retina neovascularization (formation of abnormal vessels within the retina and vitreous). These neovessels are the cause of haemorrhage, retinal detachment or even neovascular glaucoma. These are dramatic complications and finaly they can cause blindness.
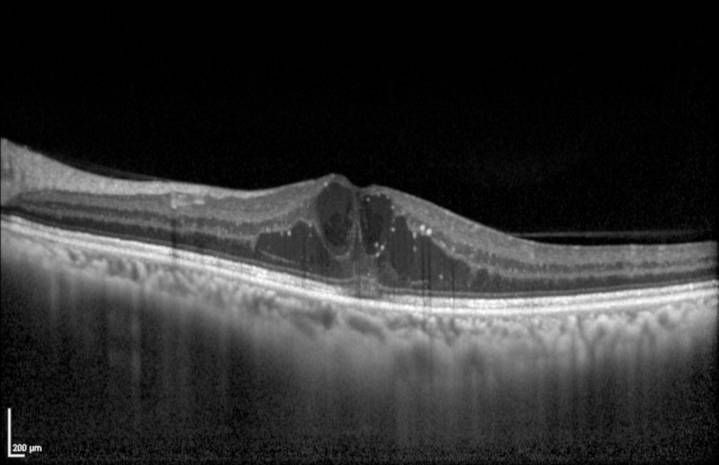
Diabetes can also affect the macula (the center of the retina). The macula is the area of the retina that can see a clear image and it is committed to central vision. At the macular level, diabetes can lead to an abnormal accumulation of fluid, which is called macular edema. Macular edema is the cause of vision loss.
Diagnosis
For a long time, diabetic retinopathy is asymptomatic. This is why it is essential for all diabetic patients to have their fundus periodically examined.
The diagnosis of diabetic retinopathy is usually based on fundus examination. Other examinations may be necessary to evaluate the severity of diabetic retinopathy such as OCT (optical coherence tomography), angiography or even OCT angiography.
OCT is today essential for the diagnosis of diabetic macular edema.
Evolution
Diabetic retinopathy is classified into different stages:
- Non proliferative diabetic retinopathy (NPDR): Mild, moderate or severe stage. Characterized by various degree of microaneurysms, haemorrhages and dilated and tortuous veins.
- Proliferative diabetic retinopathy (PDR): presence of vitreo-retinal neovascularisation.
- Diabetic ophthalmopathy: neovascular glaucoma, tractional retinal detachment, vitreous haemorrhage.


Therapy
A strict balance of glycaemic levels and of blood pressure are essential to avoid worsening of retinopathy and is beneficial in reducing disease progression rate.
- Laser treatment (pan retinal photocoagulation) is a preventive treatment in case of severe non proliferative diabetic retinopathy or proliferative retinopathy. The goal is to induce regression of existing neovascular tissue by burning ischemic retinal area. Several sessions are necessary in accordancewith the severity of the disease.
- A surgical treatment (vitrectomy) is indicated in case of intra-vitreous bleeding or in case of retinal detachment.
Regarding macular edema , intravitreal injections of corticosteroids or anti-VEGF are now the standard of care.
You can make an appointment with one of the Ophthalmologists of the department who provide specific care dedicated to this pathology:

Dr Alexandra MiereUniversity Lecturer – Staff Physician
















